
Chapter 1. Chapter 30: Reproductive System
1.1 Introduction


Welcome to the Interactive Study Guide for Chapter 30: Reproductive System! This Study Guide will help you master your understanding of the chapter's Driving Questions, using interactive Infographics and activities, as well as targeted assessment questions. Click "Next" to get started, or select a Driving Question from the drop-down menu to the right.
Too Many Multiples?
The birth of octuplets raises questions about the fertility business
DRIVING QUESTIONS
- What is the anatomy of the male and female reproductive tracts?
- What hormones participate in reproduction, and how do they work?
- What are the different types of assisted reproduction, and how do they work?
1.2 Driving Question 1:
Driving Question 1
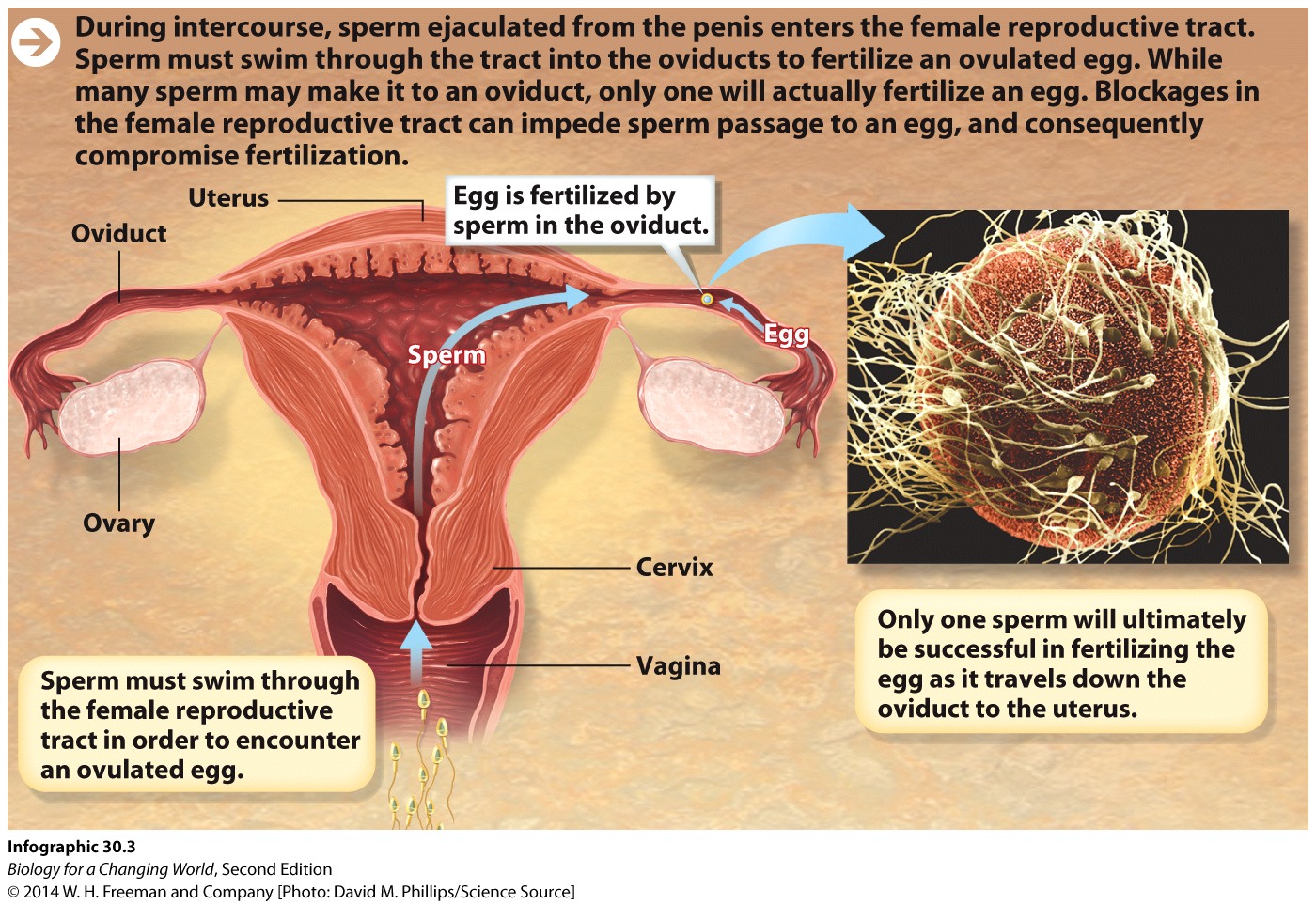
What is the anatomy of the male and female reproductive tracts?
Why should you care?
Considering how much of our sense of self is connected to our gender, it's surprising how little many people know about the human reproductive system and their own body. Understanding what the reproductive organs do and where they are is the first step toward taking an active role in your reproductive health. Even if you are not a woman, it important to understand the female reproductive system, if only because it will give you more empathy with 50% of the people you encounter every day.
The male reproductive system is based on the female reproductive system; if no androgen hormones are present in a human with X and Y chromosomes, that human will most likely develop the reproductive features of a female. If you consider this fact, it is easier to understand the male reproductive system. For example, if you consider that the testes and vasa deferentia (pl. of vas deferens) are analogous to the ovaries and oviducts in women, the roundabout route that the vas deferens makes from testis to urethra makes a little more sense. Overall, the reasons for learning about the male reproductive system are the same as for the female reproductive system: you should know how each system works both to control your reproductive health and to be sympathetic with the health concerns of all sexes.
A fertile man produces millions of sperm cells per day. The image of sperm racing each other toward the egg has become a trite joke, but it is grounded in truth. Of the vast number of sperm ejaculated, only the strongest hundred or fewer survive the race to the egg, and only one will fertilize it. Understanding how fertilization works and where it occurs is important knowledge for any responsible adult.
What should you know?
To fully answer this Driving Question, you should be able to:
- Identify and differentiate between the main parts of the female reproductive system.
- Identify and differentiate between the main parts of the male reproductive system.
- Describe the events that lead to fertilization.
Infographic Focus
The Infographics most pertinent to the Driving Question are 30.1 to 30.3 and 30.7.
Test Your Vocabulary
Choose the correct term for each of the following definitions:
| Term | Definition |
|---|---|
| A class of sex hormones, including testosterone, that is present in higher levels in men than in women and causes male-associated traits like deep voice, growth of facial hair, and defined musculature. | |
| The mixture of fluid and sperm that is ejaculated from the penis. | |
| A female sex hormone produced by endocrine cells in the ovaries (particularly in the cells of the corpus luteum) that prepares and maintains the uterus for pregnancy. | |
| Paired female reproductive organs; the ovaries contain eggs and produce estrogen and progesterone. | |
| Tubes in which sperm mature and are stored before ejaculation. | |
| The fusion of an egg and a sperm. | |
| Paired male reproductive organs, which contain sperm and produce androgens, primarily testosterone. | |
| A female sex hormone produced by the ovaries. | |
| Coiled structures that constitute the bulk of the testes and in which sperm develop. | |
| A tube that connects the bladder to the genitals and carries urine out of the body. In males, the urethra travels through the penis and also carries sperm. | |
| The muscular organ in females in which a fetus develops. | |
| The first part of the female reproductive tract, extending up to the cervix; also known as the birth canal. | |
| The sac that holds the testes. | |
| The tube connecting an ovary and the uterus in females. Eggs are ovulated into and fertilized within the oviducts. | |
| The opening or neck of the uterus, where sperm enter and babies exit. | |
| The lining of the uterus. | |
| One of a pair of tubes that carry sperm from the testes to the urethra. | |
| The primary male sex hormone, which stimulates the development of masculine features and plays a key role in sperm development. |
Identify and differentiate between the main parts of the female reproductive system.
1.
In the table below, match each organ of the female reproductive system to its function. Then match the organ to its corresponding letter on Infographic 30.1.
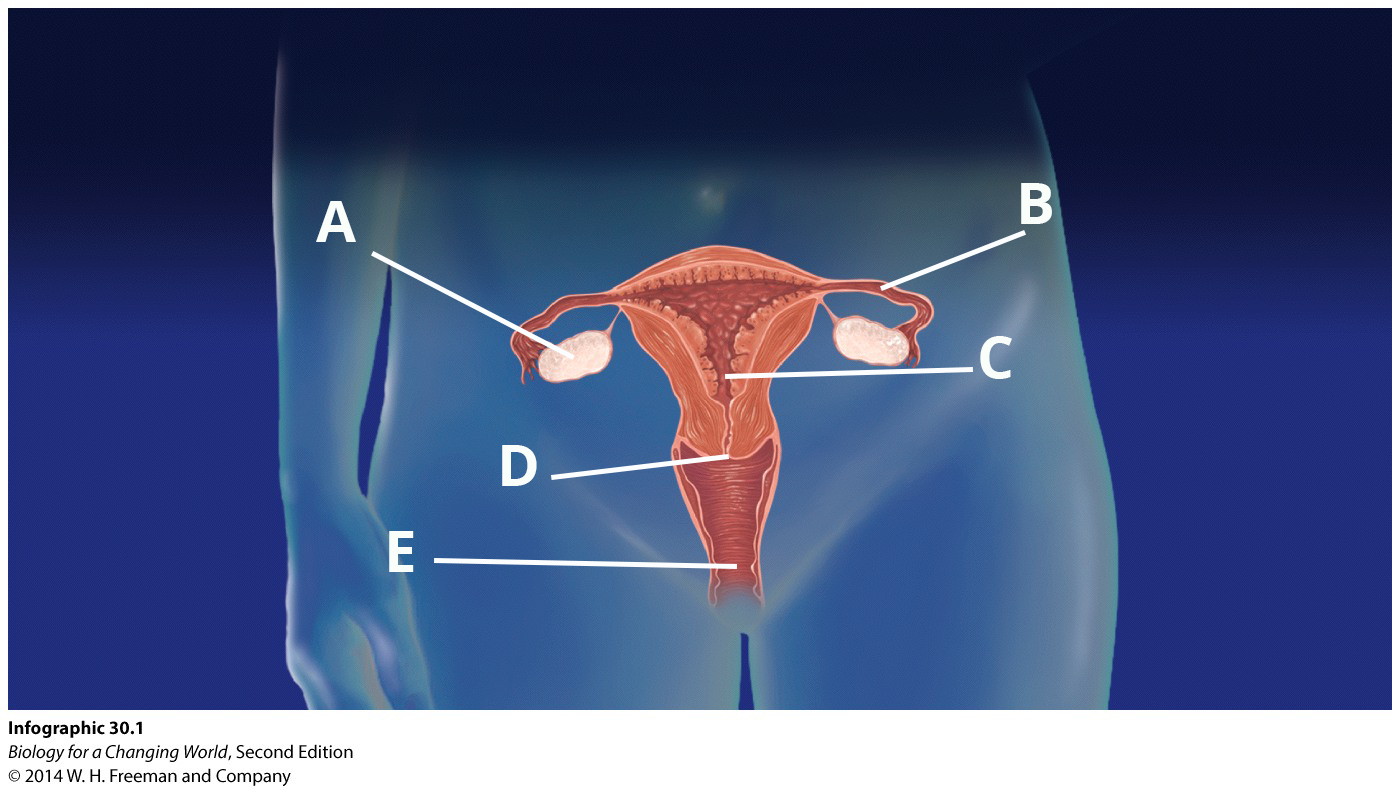
| Functions | Organs | Location |
|---|---|---|
| produces eggs and some sex hormones | ||
| site of embryo implantation and fetal development | ||
| controls passage of sperm as they travel to the egg | ||
| entrance to the female reproductive tract | ||
| site of fertilization and egg release |
Identify and differentiate between the main parts of the male reproductive system.
2.
In the table below, match each organ of the male reproductive system to its function. Then match the organ to its corresponding letter on Infographic 30.2.
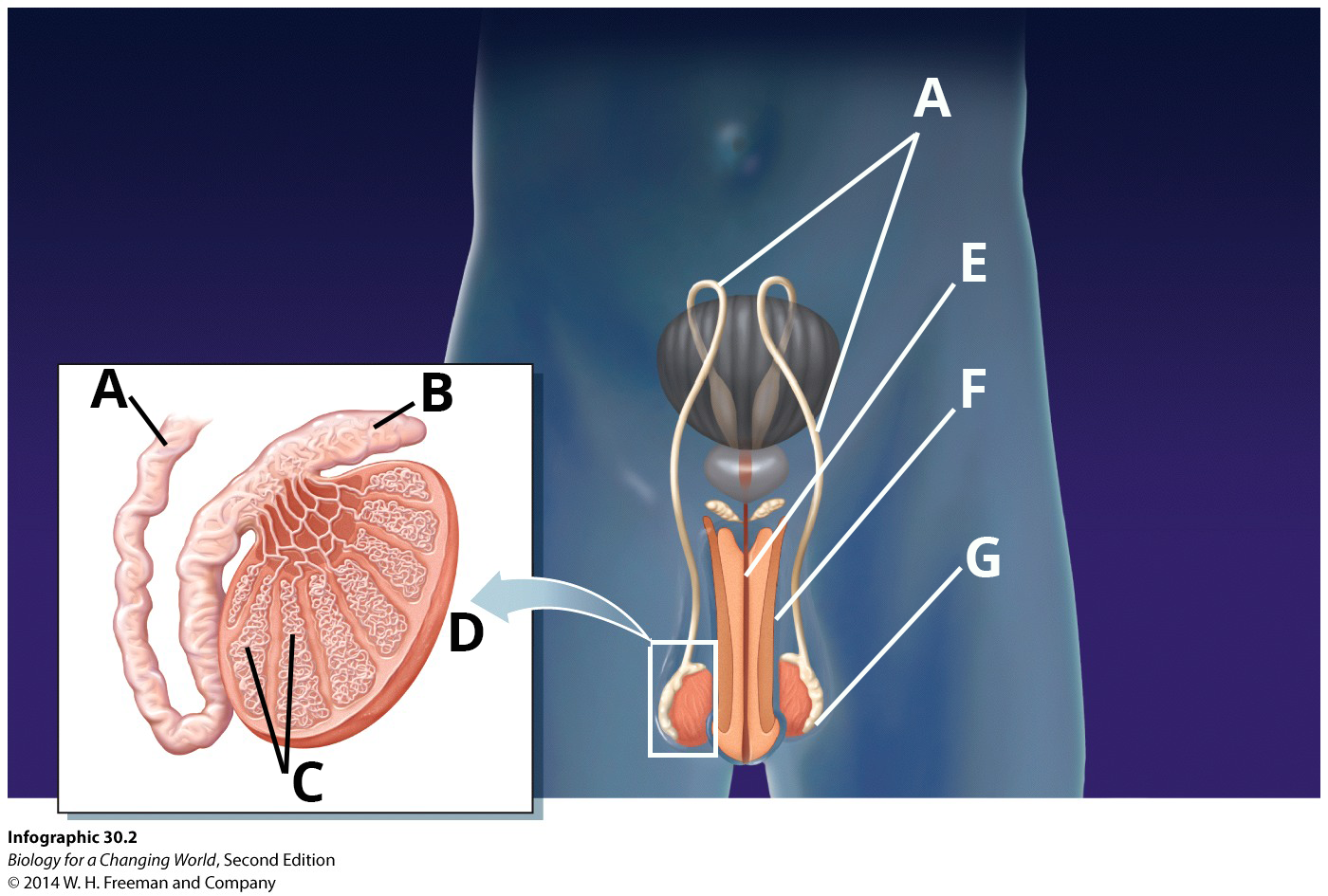
| Functions | Organs | Location |
|---|---|---|
| contains paired male sex organs | ||
| carries sperm out of body | ||
| carries sperm to the urethra | ||
| delivers sperm to the female reproductive system | ||
| stores mature sperm | ||
| ducts that are the site of sperm development | ||
| produces sperm and sex hormones |
Describe the events that lead to fertilization.
3.
What is the first step in fertilization?
4.
Assuming that a viable egg is waiting in the oviduct, what path do sperm take to reach it and fertilize it? Fill in the following boxes with the listed terms. Refer to Infographics 30.2 and 30.3 in your text.
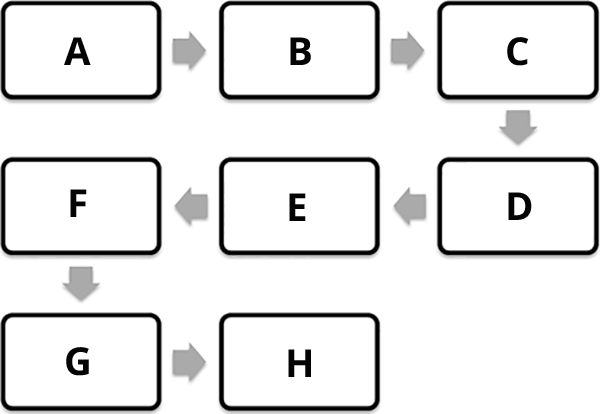
| A | |
| B | |
| C | |
| D | |
| E | |
| F | |
| G | |
| H |
Thought question: Why is it important that only one sperm fertilize the egg?
Thought question: Why is it important that only one sperm fertilize the egg?
Review Questions
5.
Normally, eggs are fertilized in the ____________, and the resulting embryos implant themselves in the ____________.
| A. |
| B. |
| C. |
| D. |
| E. |
6.
Which of these is the correct path that sperm take out of the male body?
| A. |
| B. |
| C. |
| D. |
| E. |
1.3 Driving Question 2:
Driving Question 2
What hormones participate in reproduction, and how do they work?
Why should you care?
The menstrual cycle, governed by an array of hormones, causes a predictable cycle of changes in a fertile woman's body. Chances are that you already care about the menstrual cycle, but you may not be aware of all of the changes that happen during it. Understanding the mechanics of the menstrual cycle will help you understand how fertilization occurs as well as how hormonal contraception works.
The fact that hormones support pregnancy (or perhaps prevent it) gave rise to the idea of hormone-based contraception. Imbalances in the hormones that support pregnancy are also the basis for many kinds of infertility.
What should you know?
To fully answer this Driving Question, you should be able to:
- Describe the functions and sources of the hormones that regulate the menstrual cycle.
- Explain how the ovaries, hormone levels, and endometrium thickness change throughout the menstrual cycle.
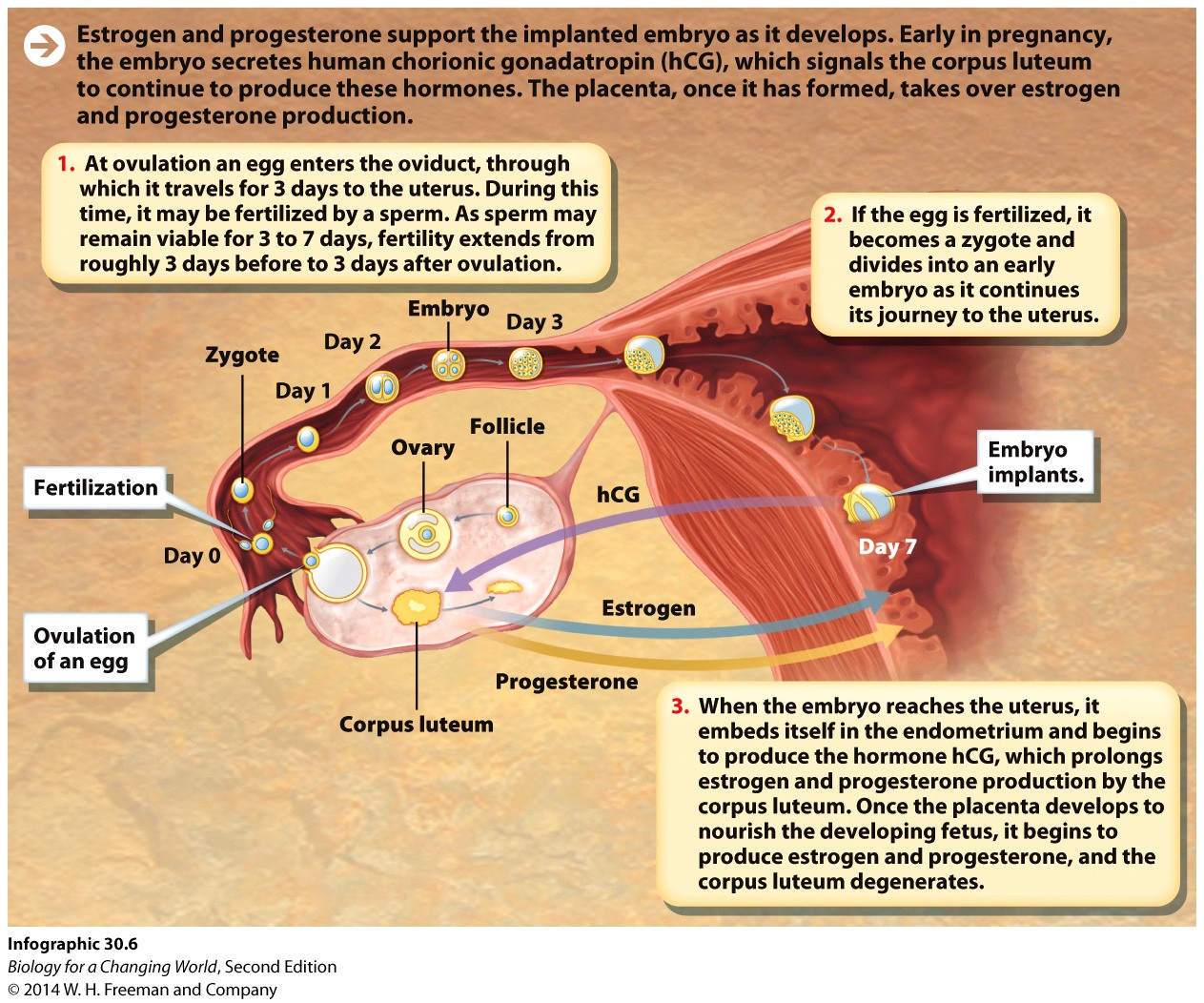
- Describe the timeline of events leading from ovulation to implantation of an embryo.
- Explain how hormones regulate pregnancy.
- Predict how hormone levels could be artificially modified to prevent pregnancy.
Infographic Focus
The Infographics most pertinent to the Driving Question are 30.5 and 30.6 and Table 30.1.
Test Your Vocabulary
Choose the correct term for each of the following definitions:
| Term | Definition |
|---|---|
| The gland in the brain that secretes luteinizing hormone and follicle-stimulating hormone. | |
| A fertilized egg. | |
| The prevention of pregnancy through physical, surgical, or hormonal methods. | |
| A female sex hormone produced by endocrine cells in the ovaries (particularly in the cells of the corpus luteum) that prepares and maintains the uterus for pregnancy. | |
| A hormone secreted by the anterior pituitary. In females, a surge of LH triggers ovulation. | |
| The stage of gestation after the eighth week after fertilization. | |
| Paired female reproductive organs; the ovaries contain eggs and produce estrogen and progesterone. | |
| A hormone secreted by the anterior pituitary. In females, FSH triggers eggs to mature at the start of each monthly cycle. | |
| The shedding of the uterine lining (the endometrium) that occurs when an embryo does not implant. | |
| A structure made of fetal and maternal tissues that helps sustain and support the embryo and fetus. | |
| An early stage of development; an embryo forms when a zygote undergoes cell division. | |
| The release of an egg from an ovary into the oviduct. | |
| A hormone produced by an early embryo that helps maintain the corpus luteum until the placenta develops. | |
| A master control region in the brain that regulates a variety of physiological functions, including hunger, thirst, temperature regulation, and reproduction. | |
| A female sex hormone produced by the ovaries. | |
| The structure in the ovary that remains after ovulation and secretes progesterone. | |
| The part of the ovary where eggs mature. |
Describe the functions and sources of the hormones that regulate the menstrual cycle.
7.
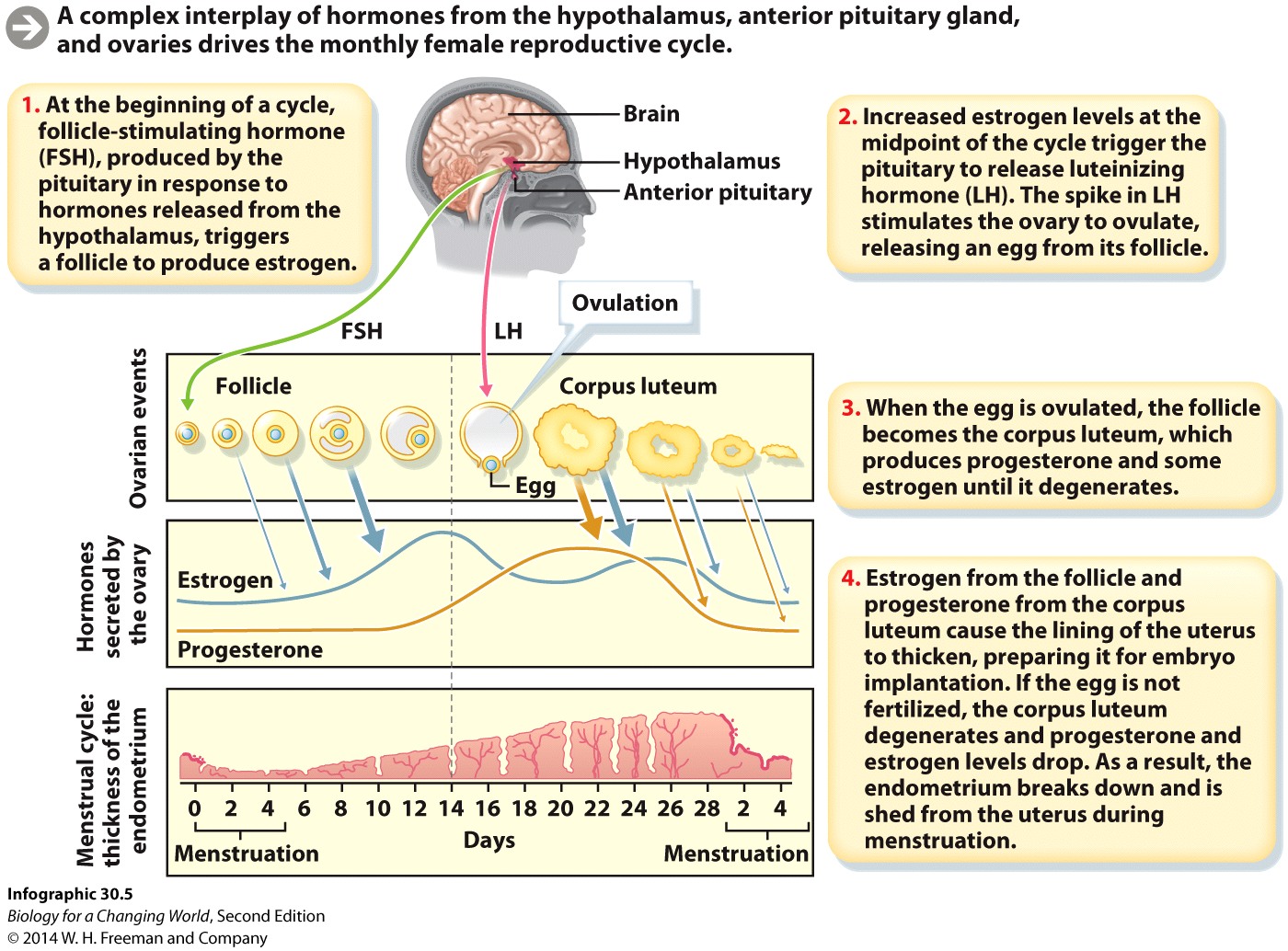
Examine Infographic 30.5 and fill in the following chart. (The first entry is an example.)
| Hormone | Where is it produced? | What does it do? |
|---|---|---|
| Gonadotropin-releasing hormone (GnRH) | Hypothalamus | Stimulates the anterior pituitary to make FSH and LH |
| FSH |
Where is it produced? |
What does it do? |
| LH |
Where is it produced? |
What does it do? |
| Estrogen |
Where is it produced? |
What does it do? |
| Progesterone |
Where is it produced? |
What does it do? |
| Hormone | Where is it produced? | What does it do? |
|---|---|---|
| Gonadotropin-releasing hormone (GnRH) | Hypothalamus | Stimulates the anterior pituitary to make FSH and LH |
| FSH | Anterior pituitary | Triggers eggs to mature at the beginning of each monthly cycle; triggers follicle to produce estrogen |
| LH | Anterior pituitary | A spike of LH causes ovulation. |
| Estrogen | Ovary (mostly produced by the follicle but some by the corpus luteum); during pregnancy the placenta produces some estrogen. | Triggers pituitary to release LH. Helps thicken the endometrium. Absence of estrogen causes the endometrium to break down and slough off. |
| Progesterone | Ovary (corpus luteum); during pregnancy, the placenta produces progesterone. | Helps thicken the endometrium. Continuing production of progesterone helps maintain pregnancy by supporting the endometrium. Absence of progesterone causes the endometrium to break down and slough off. |
Explain how the ovaries, hormone levels, and endometrium thickness change throughout the menstrual cycle.
8.
For each step in the menstrual cycle, describe what happens to estrogen levels, progesterone levels, and the endometrium.
| Time | Ovary, follicle | Estrogen levels | Progesterone levels | Endometrium |
|---|---|---|---|---|
| Days 1-14 | FSH causes a follicle to form and an egg to develop inside it. |
Estrogen levels: |
Progesterone levels: |
Endometrium: |
| Days 14-24 | LH causes release of egg, prompts follicle to become a corpus luteum |
Estrogen levels: |
Progesterone levels: |
Endometrium: |
| Days 24-28 | If a fertilized embryo does not implant in the uterus, the corpus luteum degenerates. |
Estrogen levels: |
Progesterone levels: |
Endometrium: |
| Time | Ovary, follicle | Estrogen levels | Progesterone levels | Endometrium |
|---|---|---|---|---|
| Days 1-14 | FSH causes a follicle to form and an egg to develop inside it. | Rise; peak at day 14 | Slight rise toward day 14 | Begins to thicken |
| Days 14-24 | LH causes release of egg, prompts follicle to become a corpus luteum | Declines; slight rise around day 24 | Rise; begin to decline around day 24 | Continues to thicken |
| Days 24-28 | If a fertilized embryo does not implant in the uterus, the corpus luteum degenerates. | Slight rise and then decline | Decline | At day 24 begins to slough off |
9.
What contributes to the rise in estrogen levels during days 1 to 14?
10.
What causes the peak in progesterone around day 24?
11.
What causes both progesterone and estrogen levels to begin to decline around day 26?
12.
What prevents degradation of the corpus luteum in pregnancy?
Describe the timeline of events leading from ovulation to implantation of an embryo.
13.
What has to occur for an egg to become a zygote? When does this happen?
14.
How does the zygote become an embryo? When does this happen?
15.
After fertilization, which structure, the egg, the zygote, or the embryo, actually reaches the uterus and implants in the endometrium? When does this happen?
Explain how hormones regulate pregnancy.
16.
Fill in the table with information on the hormones that support pregnancy. The location of hormone production may change, and you should note all the sources.
| Hormone | Where is it produced? | How does it support pregnancy? |
|---|---|---|
| Estrogen |
Where is it produced? |
How does it support pregnancy? |
| Progesterone |
Where is it produced? |
How does it support pregnancy? |
| HCG |
Where is it produced? |
How does it support pregnancy? |
| Hormone | Where is it produced? | How does it support pregnancy? |
|---|---|---|
| Estrogen |
Ovary (mostly by the follicle but some by the corpus luteum) Placenta |
Triggers pituitary to release LH; helps thicken the endometrium |
| Progesterone |
Ovary (corpus luteum) Placenta |
Helps thicken the endometrium; continuing production helps maintain pregnancy by supporting the endometrium. |
| HCG | Embryo | Maintains corpus luteum, stimulates it to continue to produce progesterone and estrogen until the placenta can take over production. |
Predict how hormone levels could be artificially modified to prevent pregnancy.
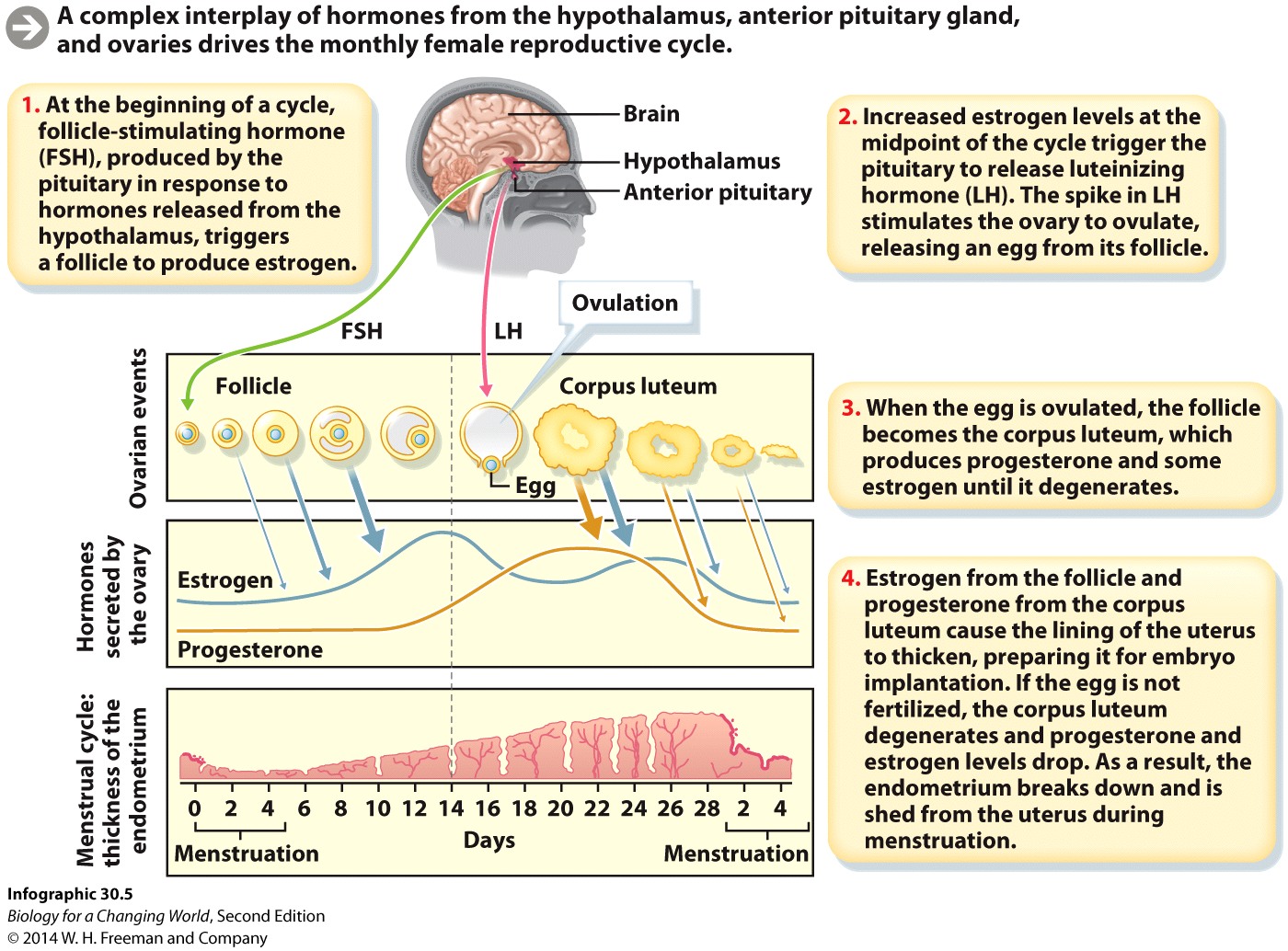
Birth control pills and other hormone-based contraceptives contain estrogen, progesterone, or both. Refer to Infographics 30.5 and 30.6 to answer these questions.
17.
How would administering progesterone and estrogen prevent pregnancy?
Review Questions
18.
Menstruation occurs when:
| A. |
| B. |
| C. |
| D. |
| E. |
19.
FSH is produced by the:
| A. |
| B. |
| C. |
| D. |
| E. |
20.
Birth control pills and other hormonal contraceptives may contain any of the following hormones EXCEPT:
| A. |
| B. |
| C. |
| D. |
| E. |
21.
A fertilized egg that has not divided (undergone mitosis) is called:
| A. |
| B. |
| C. |
| D. |
| E. |
1.4 Driving Question 3:
Driving Question 3
What are the different types of assisted reproduction, and how do they work?
Why should you care?
Infertility is a distressing issue for many couples, and diagnosing its source is complicated by the many causes of infertility. Although hopefully you will never have to face infertility, understanding its causes will teach you a great deal about your reproductive health in general.
In vitro fertilization (IVF) and intrauterine insemination (IUI) are the two main forms of assisted reproduction. Both methods have a high failure rate, but the chance of multiple births in successful procedures is much higher than the natural rate. Understanding how the procedures work will help you form informed opinions of ethical issues associated with assisted reproduction technologies.
What should you know?
To fully answer this Driving Question, you should be able to:
- Describe the causes of infertility in women.
- Describe the causes of infertility in men.
- Explain the steps of IVF.
- Compare and contrast natural fertilization with IVF.
- Compare and contrast IUI with IVF.
- Explain how IUI and IVF can both lead to multiple births.
Infographic Focus
The Infographics most pertinent to the Driving Question are 30.4, 30.8, and 30.9.
Test Your Vocabulary
Choose the correct term for each of the following definitions:
| Term | Definition |
|---|---|
| A form of assisted reproduction in which sperm are injected directly into a woman’s uterus. | |
| A form of assisted reproduction in which eggs and sperm are brought together outside the body and the resulting embryos are inserted into a woman’s uterus. |
Describe the various causes of infertility in women.
22.
The following are some of the most common causes of infertility in women:
- Hormonal imbalances
- Cancer
- Genetic problems
- Undeveloped ovarian tissue
- Endometriosis
- Polyps or fibroids
- Nonreceptive fluids
- Scarring
- Infection
Some of these causes lead to infertility through a variety of pathways: for example, one type of cancer may cause infertility through hormonal imbalance, while another causes infertility from blockages.
Come up with an organizing scheme for the different causes and decide on categories to group them in. Conditions causing blockage could be one category, but try to come up with two to four groups for the causes.
In the box, make columns for your categories. Write in the name of each category at the top of the column and list the causes with any notes you want to include about them.
|
Category: |
Category: |
Category: |
Category: |
|---|---|---|---|
|
Fill in: |
Fill in: |
Fill in: |
Fill in: |
|
Causes Blockages |
Hormonal Imbalances |
Hostile Environment for Sperm |
Nonfunctioning Organs |
|---|---|---|---|
|
Cancer Endometriosis Scarring Genetic Problems Polyps, fibroids Infections |
Cancer Undeveloped ovarian tissue Endometriosis Genetic problems Polyps, fibroids |
Nonreceptive fluids Infection |
Hormonal imbalances Undeveloped ovarian tissue Cancer Endometriosis Scarring Genetic problems |
Describe the various causes of infertility in men.
23.
The following are some of the most common causes of infertility in men:
- Hormonal imbalances
- Cancer
- Genetic problems
- Sperm abnormalities
- Prostatitis
- Testicular varicose veins
- Erectile dysfunction
- Scarring
- Infection
As with the previous question, some of these causes lead to infertility through a variety of pathways.
Come up with a categorizing scheme for the different causes and decide on categories to group them in. Try to come up with two to four groups for the causes.
In the box make columns for your categories. Write in the name of each category at the top of the column and list the causes with any notes you want to include about them.
|
Category: |
Category: |
Category: |
Category: |
|---|---|---|---|
|
Fill in: |
Fill in: |
Fill in: |
Fill in: |
|
Causes Blockages |
Hormonal Imbalances |
Erectile Dysfunction |
Sperm Abnormalities |
|---|---|---|---|
|
Cancer Testicular varicose veins Scarring Genetic Problems Prostatitis Infection |
Cancer Scarring Genetic problems |
Prostatitis Infection Cancer Scarring Hormonal imbalances |
Hormonal imbalances Testicular varicose veins Cancer Genetic problems |
Explain the steps of IVF.
24.
What is the first step in IVF, removing eggs from the ovaries, fertility drug treatment, or fertilization?
25.
Why is that the first step?
26.
What are implanted in the woman's uterus, embryos or eggs? Why does this make a difference?
27.
If in vitro means "in glass," what step is IVF named for and why?
Compare and contrast natural fertilization with IVF.
28.
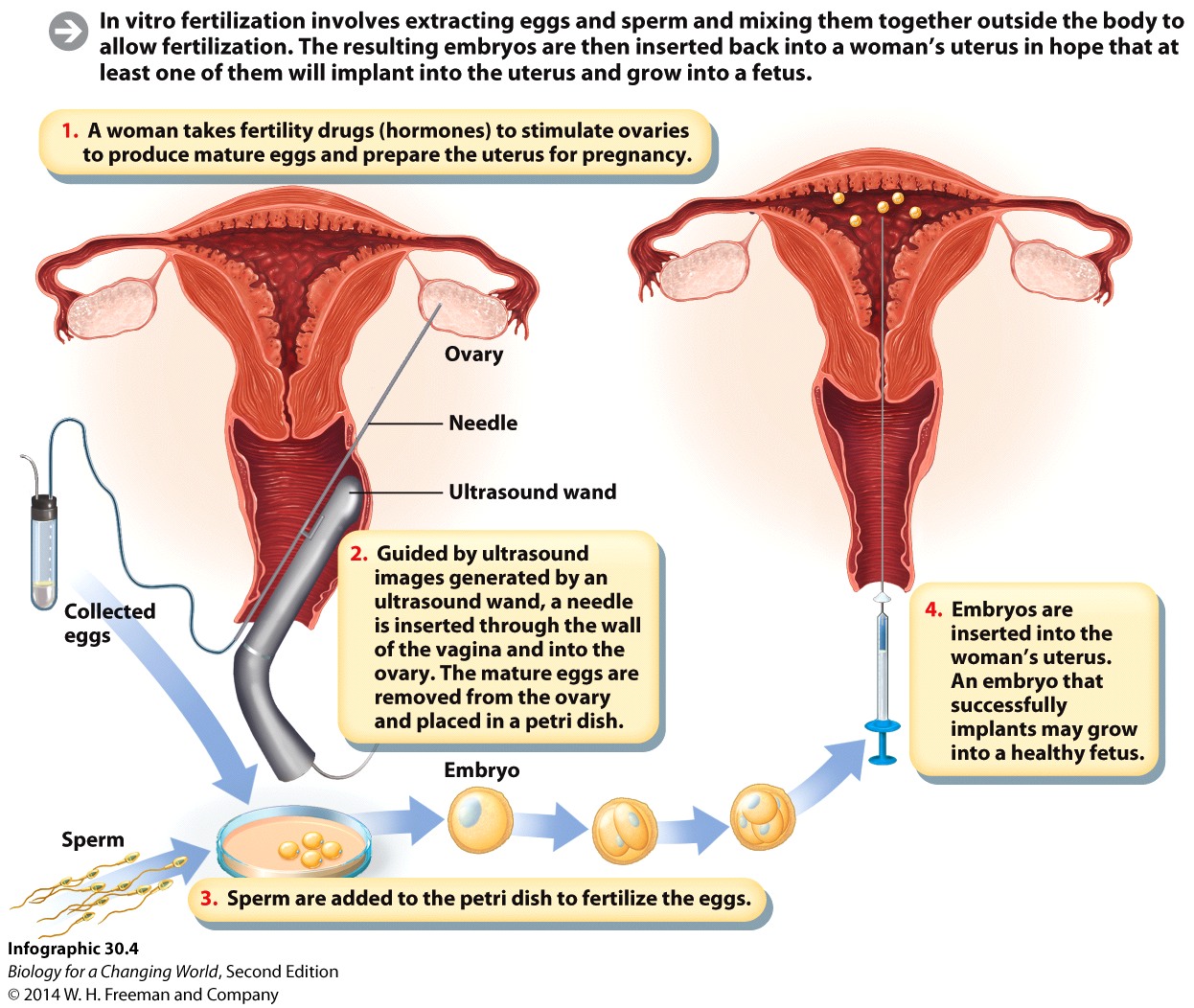
Examine Infographics 30.3 and 30.4 in your text to fill in the chart comparing natural fertilization and IVF.
| Natural Fertilization | IVF | |
|---|---|---|
| Typical number of eggs released | ||
| Where sperm fertilize egg | ||
| Number of embryos reaching uterus |
Compare and contrast IUI with IVF.
29.
What is IUI?
30.
Fill in the chart below to compare IVF with IUI.
| IVF | IUI | |
|---|---|---|
| Eggs hormonally stimulated to mature? | ||
| Ovaries hormonally stimulated to ovulate? | ||
| Eggs removed from body before fertilization? | ||
| Where does fertilization occur? | ||
| What is injected into the uterus? | ||
| Can lead to multiple births? |
Explain how IUI and IVF can both lead to multiple births.
31.
Why is the chance of multiple births much higher with IVF than with natural fertilization?
32.
Why is the chance of multiple births much higher with IUI than with natural fertilization?
33.
For which infertility procedure would it be easier to predict the number of embryos that would implant into the uterine wall? Why?
34.
What are some of the risks associated with multiple births?
Review Questions
35.
Which of the following is NOT a known cause of female infertility?
| A. |
| B. |
| C. |
| D. |
36.
In IVF eggs are fertilized ____________ and ____________ are inserted into the uterus.
| A. |
| B. |
| C. |
| D. |
37.
In IUI eggs are ____________ from the ovary and fertilized ____________.
| A. |
| B. |
| C. |
| D. |
38.
True or False: multiples conceived through natural methods do not have the same health risks as do multiples conceived through infertility treatments.
| A. |
| B. |
Activity results are being submitted...